Congestive Heart Failure (CHF) is a chronic, progressive condition that affects the heart’s ability to pump blood effectively. Over time, it can severely impact a person’s physical, emotional, and social well-being. For patients with advanced or symptomatic CHF, palliative care is increasingly recognized as an essential component of comprehensive treatment. But what exactly is palliative care for CHF, and who can benefit from it?
This article explores the role of palliative care in managing CHF, the types of patients who may need it, and how it differs from curative or life-prolonging treatments.
Understanding Palliative Care
Palliative care is a specialized form of medical care focused on improving the quality of life for people with serious, chronic, or life-limiting illnesses. It aims to relieve symptoms, reduce stress, and provide support to both patients and their families. Unlike hospice care, which is typically reserved for those nearing the end of life, palliative care can be provided alongside curative treatments and at any stage of a serious illness.
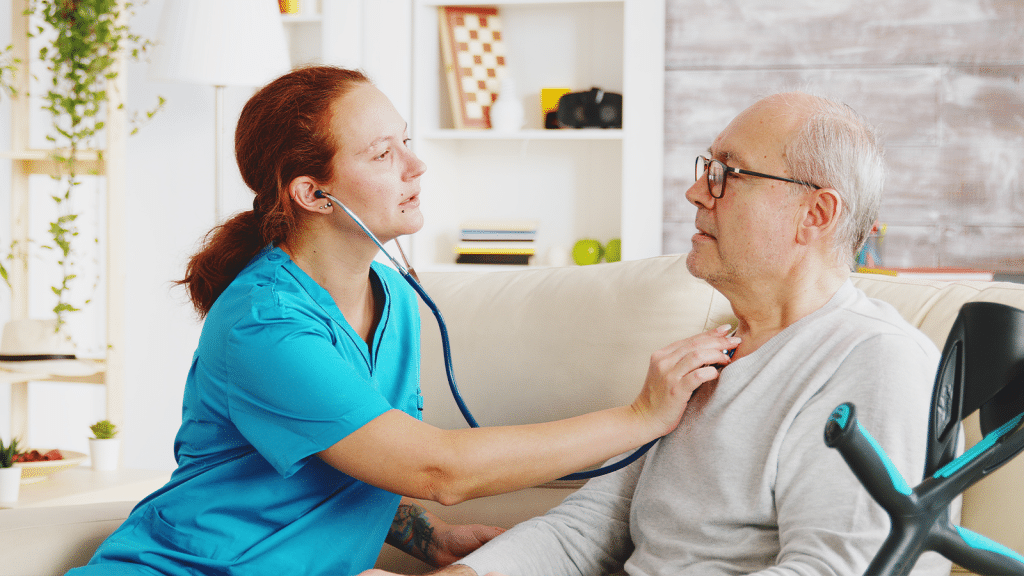
This approach is delivered by a multidisciplinary team, which may include physicians, nurses, social workers, spiritual counselors, and other healthcare professionals. The goal is holistic care — addressing physical symptoms as well as emotional, psychological, and spiritual needs.
Why CHF Patients Need Palliative Care
Congestive Heart Failure is a complex condition that can lead to significant physical limitations, emotional distress, and frequent hospitalizations. Despite advances in medical therapies and technologies, many people with CHF experience a high symptom burden that standard heart failure treatments may not fully address.
Some reasons why palliative care is especially important for CHF patients include:
1. High Symptom Burden
Patients with CHF often suffer from debilitating symptoms such as shortness of breath, fatigue, edema, chest pain, and sleep disturbances. These symptoms can be persistent and hard to manage, especially as the disease progresses. Palliative care helps in controlling these symptoms using medications, lifestyle changes, and supportive therapies.
2. Emotional and Psychological Impact
Living with CHF can lead to anxiety, depression, fear of death, and a sense of helplessness. The unpredictability of disease progression can add to psychological stress. Palliative care provides counseling, emotional support, and mental health resources to help patients cope.
3. Frequent Hospitalizations
Recurrent hospital admissions due to acute decompensations are common in CHF. These episodes disrupt life, strain healthcare systems, and often signal worsening of the condition. Palliative care aims to reduce the frequency and intensity of hospital visits through better symptom management and advance care planning.
4. Complex Decision-Making
CHF often requires decisions about interventions such as implantable defibrillators, inotropes, or heart transplants. These choices can be emotionally overwhelming and may involve ethical considerations. Palliative care teams help guide patients and families through these decisions in a compassionate and informed manner.
5. Support for Caregivers
Caring for someone with CHF can be physically and emotionally exhausting. Palliative care includes support for family members and caregivers, recognizing their crucial role in a patient’s care journey.
Key Components of Palliative Care for CHF
Palliative care for CHF focuses on comprehensive management that complements cardiology treatments. Its main components include:
1. Symptom Management
The palliative care team works to relieve symptoms such as:
- Dyspnea (shortness of breath): Managed with medications like diuretics and opioids, oxygen therapy, and positioning strategies.
- Fatigue: Addressed through energy conservation techniques and treating contributing conditions like anemia or depression.
- Pain: May stem from comorbid conditions or cardiac ischemia and is managed with analgesics or other appropriate measures.
- Depression and anxiety: Treated with counseling, medications, and relaxation techniques.
2. Advance Care Planning
This involves discussing the patient’s goals, preferences, and values related to future healthcare. It includes:
- Clarifying resuscitation preferences (e.g., CPR, intubation)
- Discussing end-of-life care options
- Preparing legal documents such as advance directives and living wills
3. Psychosocial and Spiritual Support
Addressing the mental and emotional impact of CHF is vital. Palliative care teams often include counselors and chaplains to help patients navigate grief, existential concerns, and spiritual distress.
4. Coordination of Care
Patients with CHF often see multiple specialists. Palliative care helps ensure communication between providers and facilitates continuity of care, especially during transitions between hospital and home settings.
5. Education and Communication
Effective communication is at the heart of palliative care. Patients and families are educated about the nature of CHF, what to expect as the disease progresses, and how to make informed decisions.
Who Needs Palliative Care in CHF?
While any CHF patient can benefit from palliative care, certain indicators suggest when it may be especially appropriate:
1. Advanced Heart Failure (Stage C or D)
Patients with New York Heart Association (NYHA) Class III or IV symptoms — meaning they have marked or severe limitations in physical activity — are prime candidates for palliative care. These individuals often have frequent symptoms despite optimal medical therapy.
2. Frequent Hospitalizations
If a patient has been hospitalized multiple times for heart failure exacerbations in the past year, it indicates unstable disease progression and a higher symptom burden, warranting palliative support.
3. Significant Comorbidities
Patients with other serious conditions such as kidney disease, COPD, diabetes, or dementia may find their overall health and prognosis impacted. Palliative care can help manage this complexity.
4. Declining Functional Status
A noticeable decline in the ability to perform daily activities (e.g., bathing, walking, eating) signals a need for supportive care.
5. Poor Response to Treatments
When standard therapies no longer provide relief or when the burden of treatment outweighs its benefits, palliative care can help reframe goals of care.
6. Emotional or Spiritual Distress
Patients expressing fear, hopelessness, or existential worry — especially if these feelings interfere with daily life — benefit from the counseling and support palliative care offers.
Common Myths About Palliative Care in CHF
Myth 1: It’s Only for the Dying
Palliative care is not limited to end-of-life care. It can be introduced at any stage of CHF, even early after diagnosis, to improve quality of life.
Myth 2: It Replaces Standard Treatment
Palliative care works alongside cardiology care, not in place of it. It supports the medical treatment plan by focusing on symptom relief and holistic support.
Myth 3: It Means Giving Up
Accepting palliative care is not a sign of surrender. It’s a proactive step toward living as well as possible with a serious illness.
When to Introduce Palliative Care in CHF
Ideally, palliative care should be introduced early in the course of CHF — not just when treatments stop working. An early approach:
- Enhances quality of life
- Helps patients clarify their goals
- Prevents unnecessary suffering
- Supports caregivers more effectively
Primary care providers, cardiologists, and hospital teams all play a role in recognizing when palliative care should be initiated.
Conclusion
Palliative care for CHF is about living better, not just dying well. It addresses the full spectrum of physical, emotional, and social challenges that come with heart failure. Whether newly diagnosed or dealing with advanced disease, many people with CHF can benefit from this supportive approach.
By focusing on quality of life, symptom relief, and patient-centered care, palliative care empowers individuals and their families to face CHF with dignity, knowledge, and support. As healthcare evolves to be more holistic and compassionate, integrating palliative care into CHF management is not just beneficial — it’s essential.